A) Low Back Pain (acute and persistent)
What you feel:sharp catches, “locked” sensations, morning stiffness, pain after sitting or lifting, trouble with socks/shoes.
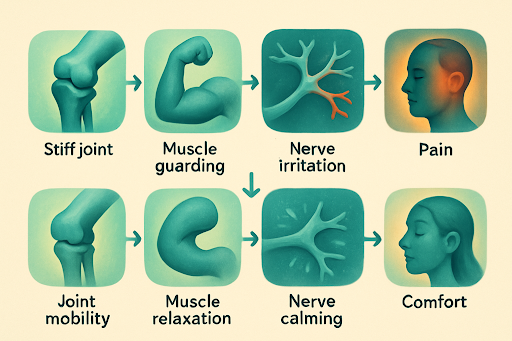
Why care helps:adjustments/mobilisations restore segmental motion; soft-tissue work reduces spasm; movement coaching builds tolerance so you can bend, lift, and sit without provoking a flare.
B) Neck Pain (desk-related, postural, or after minor strains)
What you feel:dull ache or tightness, headaches after screen time, painful rotation (checking mirrors), shoulder girdle tension.
Why care helps:cervical and thoracic adjustments/mobs improve mechanics; trigger-point release eases muscle tension; posture + strength drills handle the root drivers.
C) Sciatica (leg pain from irritated nerve roots)
What you feel:shooting/burning pain from the back or buttock down the leg, sometimes with tingling or mild weakness; often worse with prolonged sitting or certain bends.
Why care helps:improve lumbo-pelvic mechanics so the nerve is less irritated; coach positions that calmsymptoms while tissues settle; layer in nerve-glide and progressive loading when appropriate.
D) Headaches Linked to the Neck (cervicogenic) and Some Tension-Type
What you feel:one-sided head pain starting in the neck/upper back, worse with certain neck movements or postures, often with neck stiffness or tender spots.
Why care helps:treat stiff upper cervical and mid-back segments; reduce muscle tension; add ergonomics and strength work to reduce recurrence.
E) Mid-Back/Rib Pain (the “can’t take a deep breath” pinch)
What you feel:sharp, catching pain between shoulder blades or around ribs, worse with deep breaths, twisting, or carrying.
Why care helps:rib and thoracic mobilisation, breathing mechanics drills, and scapular stability work.
F) Shoulder/Hip Mechanical Pain
What you feel:limited reach, painful arcs, or hip pinch with squats or stairs.
Why care helps:restore joint play, address compensations up/down the chain (thoracic spine for shoulder; foot/pelvis for hip), then strengthen the right patterns.
G) TMJ/Jaw Tension (movement-related)
What you feel:jaw fatigue, clicking, neck/temple tension from clenching.
Why care helps:gentle joint work locally, plus neck/upper-back mechanics and stress unloading strategies.
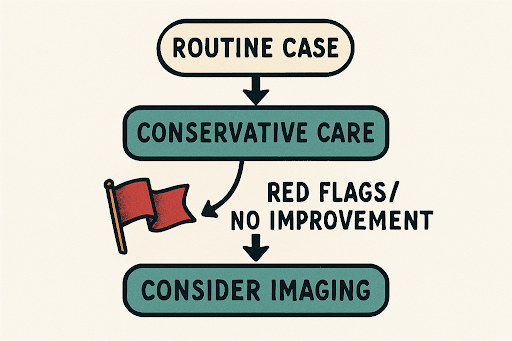
Important:In all these, the win-rate goes up when manual care + exercise + daily habit changesmove together.