Let’s start with the honest version:
You’re not crazy for asking this.
You’ve probably seen a headline like:
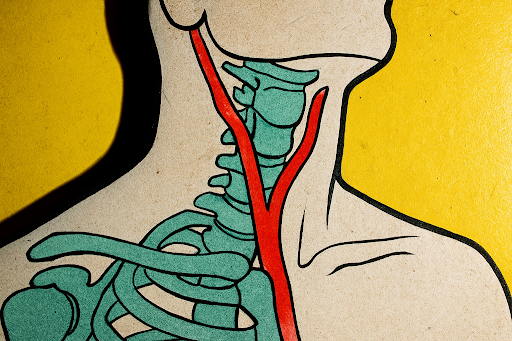
“Person goes for a neck adjustment – later has a stroke.”
…and now you’re thinking, “Hang on… am I risking my life just to fix my neck?”
So let’s sit down, have a metaphorical cup of tea, and walk through what the research actually says – not the clickbait.